Our second brain - The long-underestimated functions of the intestine

Modern cutting-edge research
Since we first became aware of the gut and its role in diseases, moods and character traits in 2017 with the book “The Psychobiotic Revolution” by Irish professor of anatomy and neuroscience John F. Cryan, the topic has never left us . As the title suggests, the research findings presented therein are nothing less than a new revolutionary thinking in medicine .
But first we would like to ask you a question. How much do you believe in human free will? Your craving for chocolate or something savory is all a matter of willpower, at least if most fitness influencers are to be believed. Your choice of partner, your sense of attractiveness, your choice of job, your moral standards, you chose all of that yourself, right?
What if your body is more of a slave to your mind than you think?
The neuroscientists at the Irish University in Cork postulate nothing less. And for a good reason. Because as the studies by Professor John F. Cryan's team show, the microbiome has more control over us than we think. The so-called vagus nerve is primarily to blame for this.
The vagus nerve
This special nerve is recognized in studies at the French University Hospital of Grenobles as a gut-brain interface ( 1. ) But who actually controls whom here? Because as it turns out, the vagus nerve is a two-way street.

But what comes from the other direction? The researchers write:
The microbiota, gut, and brain communicate in a bidirectional manner via the gut-brain axis . The vagus nerve is able to detect the metabolic products of the microbes and transmit this intestinal information to the central nervous system.
- The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis
The microbes in our intestines communicate with us and the vagus nerve serves as one of the main interfaces.
The enteric nervous system (from enteral = concerning the intestine)
Our intestines are permeated by 600 million nerve cells (for comparison: the human brain has around 100 billion nerve cells). This dense nervous system is called the “ enteric nervous system ” ( enteric from ancient Greek “enteron” for intestine)
and is therefore also referred to as “ the second brain ”.
How do our intestinal bacteria communicate with us?
Not only the enteric nervous system sends signals, but also the bacteria in our intestines themselves. Each of us has our own chemistry laboratory within us. A very individual mixture is brewed in this laboratory. Because every strain of bacteria in our intestines produces some substance. The metabolic products produced by the bacteria, such as neurotransmitters and short-chain fatty acids, reach the brain via the intestinal barrier and the vagus nerve.

There they can trigger everything from feelings of happiness to depression. If the bacteria don't get their preferred food, they can even cause illness, lack of energy and all sorts of behavior ( 2. ). But how does it work at all? Let's take a closer look at the microbiome:
How is the microbiome structured?
The microbiome consists of over 500 different bacterial species. The following 4 tribes and their respective genera make up the majority of it:

As you can see, there's a lot going on in your gut. There is also a real battle for dominance between all the bacteria. If one side gains the upper hand, it is referred to as “dysbiosis”. How does this happen? e.g. through unbalanced diet, stress or antibiotics.
How exactly do bacteria in the gut communicate with the brain?
This happens via the 3 main communication channels in the body ( 3rd - 4th ):
-
The nervous system
- Via neurotransmitters via the vagus nerve
- Via short-chain fatty acids via the vagus nerve
- The immune system
- Via cytokines via the bloodstream
- Via cytokines via the bloodstream
-
The endocrine (hormonal) system
- Via hormones via the bloodstream
The idea that bacteria talk to us perhaps sounds less absurd when you consider that all of these bacteria have been around much longer than humans themselves. We have been in symbiosis with ours throughout our entire evolution Bacteria developed in the intestines. These bacteria defend us very jealously from intruders. They fight foreign and potentially harmful microbes all on their own. Long before our immune system even comes into contact with the pathogens, our bacteria have already fought a long battle.
How our intestinal bacteria control the immune system
And they can also control the immune system itself :
Because the cells in the intestinal mucosa produce cytokines . These are alarm signals from the immune system. Cytokines and the short-chain fatty acids of the bacteria activate the microglia , which are immune cells in the brain that fight pathogens but also cause depression. ( 3. )
Some microbes, particularly the Bifido species, produce butyrate (butyric acid), which nourishes and repairs the intestinal lining. Butyrate can find its way into the brain, where it promotes a good mood, reduces inflammation or stimulates the production of a brain growth hormone. All of these changes can improve mood and even help you think better ( 4. )
The microbes themselves can also produce cytokines and communicate directly with the immune system. Bacteria of the lacto species can even produce acetylcholine and cortisol and thus dampen immune reactions .
Conditioning by intestinal bacteria?
The bacteria's communication goes so far that they can even condition us. In studies of people suffering from irritable bowel syndrome, it has been found that some lacto-species actually manipulate the opioid and cannabinoid receptors in the brain and trigger feelings of happiness in response to certain foods.
This is classic Pavlovian conditioning!
The University of Lisbon also showed in a study with fruit flies that they adapt their food choices when the microbiome changes ( 5. ).
But it has also been shown in humans that the microbiome and, accordingly, food choices change when stressed ( 6. ).
In addition, bifidobacteria, for example, have a strong influence on us via their short-chain fatty acids . A study by University College London shows that butyrate (butyric acid) in particular has an antidepressant effect on the brain ( 7. )
Each genus of bacteria seems to have their own way of asking for a proper meal, and they also have their own way of saying thank you.
Bacteroidetes especially like fat , Prevotella love carbohydrates and Bifidos prefer fiber . In return, they provide us with their positive metabolic products.
In the worst case, you can clearly see this in EHEC (enterohemorrhagic Escherichia coli), which behave well until they run out of sugar. Then the bacteria begin to eat into the intestinal lining and cause bloody diarrhea. This is where it actually helps to eat sugar!
What are short chain fatty acids?
Short-chain fatty acids are produced by certain intestinal bacteria through the fermentation of complex, resistant carbohydrates (e.g. fructo-oligosaccharides, sugar alcohols, resistant starch, inulin and polysaccharides from plant cell walls) that escape digestion and absorption in the small intestine and thus end up in the large intestine.
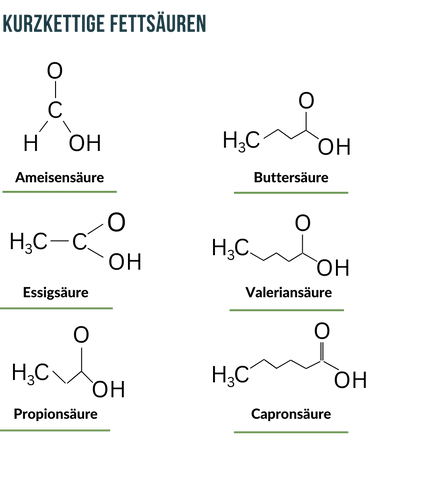
As has been found in some studies, it is precisely these short-chain fatty acids that can correct an unfavorable composition of the intestinal bacteria themselves.
Because they serve as food for those bacteria that have a particularly high protective function for the human organism: For example, they prevent inflammation and protect against an overactive immune system by maintaining the natural barrier function of the intestinal mucosa ( 8. ).

Short-chain fatty acids and energy production
But they also play an important role in the metabolism of our cells. The special fatty acid butyrate (butyric acid) is required for ATP production in the mitochondria ( 9. ). We have already written about how this works in our blog article “ How Cordyceps increases your performance ”.

Source: imd-berlin
Modern society as a result of our microbiome?
The power of bacteria over our brain is so great that researchers are even wondering whether our entire society actually serves the bacteria in our intestines rather than ourselves. Are we slaves to bacteria? The statement is very exaggerated, but in a certain sense you could say that.
The University of Oslo has impressively described the fact that even our choice of partner is influenced by our bacteria ( 10. ).
"The reproductive microbiome can exert selection pressure on males and females, which has a critical impact on sexual selection, sexual conflict, and the emergence of mating systems and reproductive barriers."
Many of your personal characteristics that you perceive as "that's just how I am" could actually be vague messages from the gut ( 2. ).
The microbiome and early childhood development
How essential the microbiome is for us can also be seen in other places.
The bifidobacterium, for example, is specialized in processing specific sugars from breast milk. The metabolic products (sialic acid, ILA (indole-3-lactic acid)) that are created are particularly important for the development of the early childhood brain. Without bifidobacteria, babies would be able to process human breast milk much more poorly ( 11. ).
A study published in the journal Cell Chemical Biology shows that
"Bifidobacterium longum has successfully adapted to the unique niche of the infant gut by producing an enzyme called LnbX (lacto-n-biosidase), which enables this microbe to grow on a sugar that is only sufficiently present in human milk."
Our bacteria also train the cells of our immune system. In newborns, the immune system is very aggressive and overactive. The immune cells do not yet know which cells and bacteria are friendly and which are hostile ( 12. ). The microbiome releases certain metabolic products that are absorbed and processed by the dendritic cells, which are regulators of the immune system. Special immune cells are then formed (T helper cells), which are only found in the intestine and allow the friendly microbes to do their thing ( 13. )
Caesarean section and substitute milk
This of course means that the unique mix of bacteria that is given to the child during a normal birth is irreplaceable. In this way, the mother passes on her (in the best cases) well-trained microbiome to the child. However, this is not the case with a cesarean section. Likewise, natural breast milk cannot yet be completely replaced.
The effect of the psyche on the microbiome
We said at the beginning that communication between the gut and the brain is a two-way street. It turns out that norepinephrine and dopamine from the brain can also cause the number of pathogenic bacteria in the intestine to skyrocket.
These are stress molecules that are triggered in “fight or flight” reactions. Their job is to make you anxious and alert. They subdue the intestines and immune system, giving pathogenic bacteria more chances to invade ( 14. )
Stress can also affect the levels of acid, mucus and other secretions in the intestines.
A study of university students who were examined before and during an exam phase showed that stress hormones even reduce the number of good microbes. Students under acute exam stress had fewer lactobacteria in their intestines than the control group ( 15. ).
Depression due to poor diet?
What is depression? There is actually hardly any difference to “sickness behavior”, i.e. normal illness behavior. The classic “pull the covers over your head and want to be alone.”
Depressive behavior has a long evolutionary history to ensure your survival during illness by conserving energy to fight the infection.
However, in the modern world with prevailing stress, diets high in fat and sugar, and sedentary lifestyles, depression is no longer a useful adaptation. This is called chronic illness behavior. This shows how a negative cycle can arise.
The fact that stress actually increases the permeability of the intestinal barrier has now also been well researched (16-18).
The important and sensitive intestinal barrier
There are some extremely important barriers in our body:
- The intestinal barrier
- the portal vein
- the blood-brain barrier.
These barriers are structured as follows:

The “tight junction” proteins are particularly important here (in German “tight connection”)
Tight junction proteins close the cell spaces in the intestinal mucosa and the other barriers. Their function is regulated not only by glycine and glutamine, but also particularly by zonulin .
Zonulin is a protein that increases the permeability of tight junctions between cells in the wall of the digestive tract.
Wikipedia
The disruption of the intestinal barrier function is also known as leaky gut . This term is translated from English and means “permeable intestine”. Zonulin can be used as a laboratory marker that indicates a disruption of the intestinal barrier.
What can you do to keep your gut healthy?
Omega 3 :
Studies in humans and animals have shown that omega-3 can influence the gut-brain axis via the composition of the gut microbiota (19.)"In our laboratory, we found that polyunsaturated fatty acids such as omega-3 reverse the effects of early childhood stress on the gut microbiota. Rats separated from their mothers are stressed, leading to disruption of gut-brain function and a "These rats show signs of depression and anxiety. However, supplementation with omega-3 fatty acids restores their microbiota and reduces cortisol levels.".
fiber
The good bifidobacteria in the intestine love fiber and metabolize it into butyrate . This helps repair the intestinal lining and releases neurotransmitters for a positive mood.
Foods high in fiber include:
- artichokes
- chicory
- Endives
- lenses
- Leek
- asparagus
- Beans - especially limas
- Onions
- Garlic
- Bananas, apples, oranges
- Beetroot
- broccoli
- fennel
- Ginger
Resistant starch
is caused by cooling cooked, starchy foods such as potatoes, rice and pasta. When starch cools, it changes its chemical structure . It becomes almost indigestible for the intestines . It may sound unhealthy at first, but it remains intact for the intestinal bacteria and has a positive influence on the intestinal flora.
Ferments
Fermented foods contain live bacteria that have a positive effect on the intestines. The selection of fermented foods is large:
Whether it's kimchi, sauerkraut, kombucha, tempeh, the normal salt and dill pickles from the supermarket (important: don't use "cornichons" or other pickled cucumbers, they always have sugar and brandy vinegar added), kefir or yoghurt, there's hardly any excuse no longer eating ferments. However, be careful if you have histamine intolerance or chronic inflammatory bowel disease.
yogurt
When it comes to yoghurt, you should make sure that it has no flavor, no sugar or additives. Also: the greasier the better!
When you remove the fat from dairy products, you concentrate the milk sugar, which changes the relationship between the lactobacteria and the sugars they like to eat. It was shown that the antidepressant properties of the microbes only develop from yogurt with a higher fat content ( 20. ).
Research also shows that vitamin D enhances this effect of the active microbes in yogurt ( 21. ).
Antioxidants
Antioxidants can increase the levels of healthy bifido and lacto species. They generally strengthen gut health and can improve inflammatory bowel disease ( 22. ).
A2 milk
BCM-7 from A1 milk binds to opioid receptors throughout the body. This makes it addictive. In the intestine, BCM-7 can promote inflammation and delay intestinal transit . Due to the changed structure of A2 milk, BCM-7 cannot be split off in the first place. We also wrote about this in our article on A2 casein .
Functional mushrooms:
Reishi (Ganoderma Lucidum)
Supplementation with G. lucidum polysaccharide strain S3 (GLPS3) increased the relative abundance of the beneficial bacteria such as Lactobacillus, Roseburia and Lachnospiraceae. GLPS3 inhibited pancreatitis by regulating the microbiota in one study ( 23 ).
Chaga (Inonotus obliquus)
Chaga can cause changes in the microbiome and bring the numbers of Bacteroidetes towards a healthy bacterial profile. An experiment was carried out with three different dosages of Chaga extract: 0.1, 0.2 and 0.4 g/kg/day ( 24 - 25 ).
Turkey Tail (Trametes versicolor)
One study reported that Turkey Tail fungus modifies Bifidobacteria and Lactobacillus, thereby regulating the human microbiome ( 26. )
Another study also reported that polysaccharides from Trametes versicolor can alter bacterial flora. In this experiment, healthy people were used for a clinical study. They received 1200 mg three times daily on an empty stomach on days 1 to 14.
The results of the study say that Turkey Tail regulates the composition of the microbiome, which was not the case in the control group ( 27 ).
What should you avoid for a healthy gut?
Highly processed foods
A large Norwegian study of 23,000 women and children has shown that highly processed foods can trigger depression and anxiety, likely by allowing the worse bacteria to grow in the gut. The highlight: The children themselves ate normally, but the children of mothers who ate junk food during pregnancy were more likely to have psychological problems ( 28. ).
Another study from Norway with 5,700 participants showed a direct link between a poor diet and depression and anxiety ( 29 - 30 ).
Minimize sugar consumption
Many intestinal bacteria that like sugar belong to the pathogenic species.
A large international study has also demonstrated a significant association between sugar consumption and depression ( 31 ).
Drink less alcohol
In another study from the University of Cork, rats were exposed to alcohol vapor to measure the responses of the microbiome. After 4 weeks, the feces were analyzed, in which the diversity of the microbiota decreased significantly and the number of pathogens increased. This is also consistent with other studies that have made similar discoveries ( 32. ).
Emulsifiers
Emulsifiers are used to mix oil and water. There are enough examples of this in nature. However, some industrial emulsifiers pose a problem as they can have negative effects on the intestines. Two of them, carboxymethycellulose (CMC) and polysorbate 80 (P80), were shown in one study to reduce the thickness of the important mucus layer in the intestine and the diversity of the microbiome ( 33. ).
In mouse studies, the emulsifiers have also led to obesity and colitis. Studies on humans are currently being carried out.
The natural emulsifier lecithin, on the other hand, has no effect.
Attention: These two emulsifiers are often used for gluten-free products .
Unlike studies in which unrealistically high amounts of a substance are used, these studies explicitly looked at the smallest amounts, down to 1/10 of the content that may be freely sold in products.
So how come such products are allowed? Because most testing sites such as the FDA in the USA or the EMA in Europe do not look for a potentially negative influence on the microbiome ( 34. ).
Overweight
People who are overweight or obese suffer varying degrees of dysbiosis, which leads to chronic inflammation. Weight loss balances the microbiota, reduces inflammation and improves mood. The balance of intestinal bacteria can help you lose weight ( 35. - 36. )
Finally:
The whole field is cutting-edge research and there are still many mechanisms that are unclear. In addition, many observations are based on animal studies.
However, there are still more similarities between animals and humans than differences, and several of the studies have shown that most human microbes function as expected when transferred to mice.
Sources:
-
https://www.frontiersin.org/articles/10.3389/fnins.2018.00049/full
The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis
-
https://pubmed.ncbi.nlm.nih.gov/22968153/
Mind-altering microorganisms: the impact of the gut microbiota on brain and behavior
-
https://pubmed.ncbi.nlm.nih.gov/14744800/
Regulation of microglial inflammatory response by sodium butyrate and short-chain fatty acids
-
https://pubmed.ncbi.nlm.nih.gov/21785220/
Fatty acid-induced gut-brain signaling attenuates neural and behavioral effects of sad emotion in humans
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3877687/
A holistic medium for Drosophila melanogaster
- https://pubmed.ncbi.nlm.nih.gov/11139006/
Stress and food choice: a laboratory study
- https://pubmed.ncbi.nlm.nih.gov/27346602/
The neuropharmacology of butyrate: The bread and butter of the microbiota-gut-brain axis?
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3337124/
The role of gut microbiota in immune homeostasis and autoimmunity - https://academic.oup.com/ibdjournal/article/23/1/2/4595517
An Overview of the Innate and Adaptive Immune System in Inflammatory Bowel Disease -
https://www.sciencedirect.com/science/article/pii/S0169534719303258
The Reproductive Microbiome: An Emerging Driver of Sexual Selection, Sexual Conflict, Mating Systems, and Reproductive Isolation - ScienceDirect -
https://pubmed.ncbi.nlm.nih.gov/22688187/
The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner
-
https://pubmed.ncbi.nlm.nih.gov/21937990/
Peripheral education of the immune system by colonic commensal microbiota
-
https://www.nature.com/articles/ncomms14715
CD40-signaling abrogates induction of RORγt+ Treg cells by intestinal CD103+ DCs and causes fatal colitis
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1489335/
Enhancement of In Vitro Growth of Pathogenic Bacteria by Norepinephrine: Importance of Inoculum Density and Role of Transferrin -
https://pubmed.ncbi.nlm.nih.gov/18023961/
Investigating the role of perceived stress on bacterial flora activity and salivary cortisol secretion: a possible mechanism underlying susceptibility to illness -
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4604320/
Breaking down the barriers: the gut microbiome, intestinal permeability and stress-related psychiatric disorders -
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7213601/
Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition -
https://www.frontiersin.org/articles/10.3389/fimmu.2020.01823/full
Psychological Stress, Intestinal Barrier Dysfunctions, and Autoimmune Disorders: An Overview -
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5751248/
Impact of Omega-3 Fatty Acids on the Gut Microbiota
-
https://pubmed.ncbi.nlm.nih.gov/27466606/
Intake of High-Fat Yogurt, but Not of Low-Fat Yogurt or Prebiotics, Is Related to Lower Risk of Depression in Women of the SUN Cohort Study
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3085575/
Gut Microbiota, Probiotics, and Vitamin D: Interrelated Exposures Influencing Allergy, Asthma, and Obesity?
-
https://pubmed.ncbi.nlm.nih.gov/21151942/
Anti-inflammatory effects of resveratrol, curcumin and simvastatin in acute small intestinal inflammation -
https://pubmed.ncbi.nlm.nih.gov/27616696/
Effects of Ganoderma lucidum polysaccharides on chronic pancreatitis and intestinal microbiota in mice
-
https://pubmed.ncbi.nlm.nih.gov/28197985/
Inonotus obliquus polysaccharide regulates gut microbiota of chronic pancreatitis in mice
-
https://pubmed.ncbi.nlm.nih.gov/25861415/
Ethanol extract of Innotus obliquus (Chaga mushroom) induces G1 cell cycle arrest in HT-29 human colon cancer cells
-
https://pubmed.ncbi.nlm.nih.gov/25006989/
Effects of polysaccharopeptide from Trametes versicolor and amoxicillin on the gut microbiome of healthy volunteers: a randomized clinical trial
- https://pubmed.ncbi.nlm.nih.gov/23435630/
Trametes versicolor extract modifies human fecal microbiota composition in vitro
-
https://pubmed.ncbi.nlm.nih.gov/26109579/
High glycemic index diet as a risk factor for depression: analyzes from the Women's Health Initiative
-
https://pubmed.ncbi.nlm.nih.gov/24074470/
Maternal and early postnatal nutrition and mental health of offspring by age 5 years: a prospective cohort study
-
https://pubmed.ncbi.nlm.nih.gov/21715296/
The association between habitual diet quality and the common mental disorders in community-dwelling adults: the Hordaland Health study
-
https://pubmed.ncbi.nlm.nih.gov/12415536/
A cross-national relationship between sugar consumption and major depression?
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5518606/
Drunk Bugs: Chronic Vapor Alcohol Exposure Induces Marked Changes in the Gut Microbiome in Mice
-
https://pubmed.ncbi.nlm.nih.gov/25887492/
Keeping good lining at bay: impact of emulsifiers
- https://pubmed.ncbi.nlm.nih.gov/25869573/
Metabolism: Dietary emulsifiers--sweepers of the gut lining? -
https://pubmed.ncbi.nlm.nih.gov/21897203/
Behavioral satiety sequence in a genetic mouse model of obesity: effects of ghrelin receptor ligands
-
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4010744/
Impact of the gut microbiota on the development of obesity and type 2 diabetes mellitus
-
https://pubmed.ncbi.nlm.nih.gov/25846319/
Gut Microbiota: The Conductor in the Orchestra of Immune-Neuroendocrine Communication
-
https://www.frontiersin.org/articles/10.3389/fpsyt.2022.815422/full
Fecal Microbiota Transplantation (FMT) as an Adjunctive Therapy for Depression—Case Report
-
https://pubmed.ncbi.nlm.nih.gov/25082483/
Transfer of gut microbiota from lean and obese mice to antibiotic-treated mice
-
https://pubmed.ncbi.nlm.nih.gov/27491067/
Transferring the blues: Depression-associated gut microbiota induces neurobehavioral changes in the rat
-
https://pubmed.ncbi.nlm.nih.gov/16945350/
Antidepressant-like effects of the histone deacetylase inhibitor, sodium butyrate, in the mouse
-
https://www.sciencedirect.com/science/article/pii/S0960982220310691
Enduring Behavioral Effects Induced by Birth by Caesarean Section in the Mouse
-
https://pubmed.ncbi.nlm.nih.gov/34041591/
Cesarean delivery and risk of hospitalization for autoimmune disorders before 14 years of age
-
https://pubmed.ncbi.nlm.nih.gov/26371844/
Cesarean section and disease associated with immune function
0 comments







